If I told you that a half-day training program creates life-changing benefits for women and their families, I’d understand if you were skeptical. Yet, implausible as that sounds, researchers at the University of California San Francisco Bixby Center have shown precisely how it can happen. And it’s a story that deserves to be shared.
Let’s start with the world as we know it. When a woman in the U.S. asks her doctor about contraception, she’ll usually get a prescription for birth control pills or a recommendation that her partner use condoms. This has been the practice for many decades, despite the development of far more effective and convenient forms of birth control—the IUD and the contraceptive implant.
Although long-acting reversible methods of contraception, or LARCs, have been proven to be highly effective and safe for women of all ages, whether they have had children or not, most women don’t hear about them from their doctors because of outmoded beliefs that these methods are appropriate for older married moms. Providers shy away from routinely offering LARCs because they may lack confidence in their ability to insert the devices correctly and clinic routines may not accommodate slightly longer visits. Even unfamiliarity with the right billing codes can prevent a woman from getting the most effective form of birth control—a particularly crucial issue now that the Affordable Care Act covers all methods.
These barriers to good care have bad consequences: Only 9 percent of women in the U.S. use LARCs, while they are much more popular in other industrialized countries. And because women who depend on pills and condoms are much more likely to get pregnant by accident than women who use long-acting methods, low use of the most effective birth control is partially responsible for the fact that half—yes, you read that right: half—of all pregnancies in this country are unintended.
Now: let’s create a better world. A few years ago, a team of researchers at the University of California San Francisco, led by Cynthia Harper, decided to do something about this problem. The UCSF team developed a half-day training program to update physician knowledge and to train all clinic staff about the relative benefits and risks of different contraceptives, with a focus on LARCs. The aim was to raise the knowledge level about the most effective birth control methods—and the hope was that this would lead not only to more women using these methods, but eventually to fewer women being surprised by a pregnancy they had been trying to avoid. The training was distinguished by its use of up-to-date medical evidence, and by a comprehensive clinic-wide approach: everyone from schedulers to billing clerks to the doctors themselves learned about how to integrate underused contraceptives into their practice.
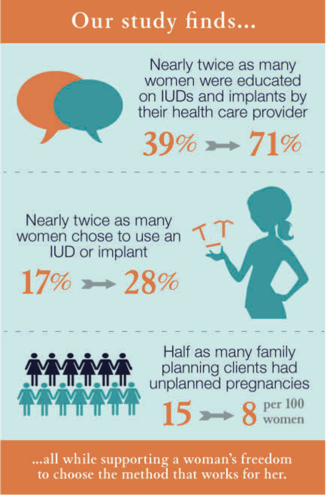
The results, appearing in the Lancet this week, are impressive. They show for the first time how a clinic-based intervention can decrease unintended pregnancy. The researchers found, first, that in clinics where the training had been conducted, 71 percent of women were informed about LARCS, compared to 39 percent in the business-as-usual clinics. Second, in clinics where personnel had been trained, 28 percent of women coming in for a family planning visit chose an IUD or an implant, compared to 17 percent of comparable women in other clinics. Third, and most remarkably, the training halved the number of unintended pregnancies.
Bottom line: a short and relatively inexpensive training of health care providers dramatically reduces the emotional, physical, and societal costs of unintended pregnancy.
That, my friends, is true value for money.